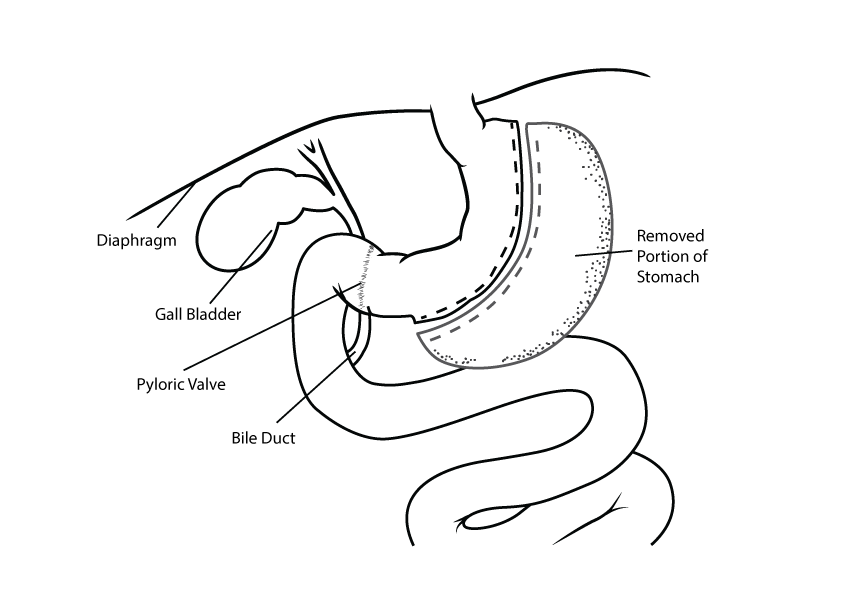
Laparoscopic Sleeve Gastrectomy
Laparoscopic sleeve gastrectomy is a restrictive procedure that is performed via 5 small key-hole incisions on your upper abdomen. During the procedure 70-80% of the stomach is removed leaving a new small tube-shaped stomach that has the capacity of approximately half a cup or 125mls. Sleeve gastrectomy works by creating a restriction on portion size, this is opposed to gastric bypass surgery that also incorporates a malabsorptive component to weight loss. After sleeve gastrectomy a balanced diet is consumed only in much smaller quantities. If this strict portion control was attempted without surgery hunger would sabotage long-term success. Sleeve gastrectomy works by removing the Ghrelin producing cells of the stomach which greatly reduces appetite and allows satiety to be quickly achieved.
Weight Loss Outcomes
Many long-term studies show an excess weight loss of 60% at 5 years after sleeve surgery (excess weight is how many kilograms you are over the body weight you would be if you had BMI 25). Patients also see improvement in diabetes, hypertension, dyslipidemia, obstructive sleep apnea and degenerative joint disease. Life after sleeve gastrectomy includes the benefits of moving more freely, improved sleep, improved mood and increased energy.
As sleeve surgery has been shown to reverse diabetes and hypertension a plan should be established with your surgeon, GP and medical specialist to reduce medication as your weight decreases. Bariatric surgery also improves fertility with high rates of reversal of PCOS (polycystic ovarian syndrome). A safer pregnancy is experienced with the reduced risk of pre-eclampsia, gestational diabetes, induced labour, post-partum haemorrhage, c-section and epidural complications.
Sleeve gastrectomy was first performed in America in the late 1980’s to reduce weight in patients going for gastric bypass who were to obese for the operation to be completed safely. It has since gained widespread popularity due to its safety profile and reliable outcomes. Sleeve gastrectomy has a a lower risk of bleeding, leak and subsequent re-operation compared to gastric bypass. As a large portion of the stomach is removed from your body the operation can not be reversed. It is also safer from a nutritional point of view as bypass causes malabsorption of nutrients with deficiencies in Calcium, Iron and Vitamin B12 commonly seen.
The safest approach is to have your operation performed by a specialist bariatric surgeon who is contributing to our national peer reviewed data registry. A detailed explanation of the risks of surgery should be outlined in your initial appointments including strategies to prevent and treat known complications. Post-operative care is paramount with support from dieticians, physiotherapists and psychologists leading to improved long-term success.
- Routine blood panel: full blood count, kidney function, liver function, clotting factors, thyroid
- Barium swallow test- to screen for GERD (gastro-esophageal reflux disease) and hiatus hernia.
- Upper abdominal ultrasound- to check liver size and presence of gallstones.
- Liver shrink diet- to reduce the volume of your liver so the surgery can be performed safely, this is a shakes based Very Low Calorie Diet such as Optifast, Optislim or KicStart, for most patients it ranges between 2-6 weeks depending on your BMI and liver size.
- The procedure is performed under general anaesthesia and takes approximately 1 hour.
- It begins with separating the stomach away from the fatty apron that is attached along it’s length called greater omentum
- The patient is then checked for a hiatus hernia and if one is present a repair is carried out to prevent GERD.
- A calibration tube also called a bougie is then inserted down the esophagus into the stomach to act as a guide ensuring the correct amount of stomach is removed.
- A stapling and cutting device is used to divide the stomach in a vertical fashion along its entire length creating the new tube shaped sleeve. The excess stomach is removed from the abdominal cavity via one of the keyholes and is routinely sent to the pathology lab to be examined before disposal
- Shoulder tip gas pain is common after laparoscopic surgery and will subside within 48 hours, key-hole wounds should not be painful when managed with simple analgesia such as paracetamol.
- Nausea can be an issue in the days after surgery and you will be provided with a script for anti-emetics to allow adequate hydration.
- The first two weeks after surgery involve a liquid diet while the long wound in the stomach heals and swelling subsides.
- In weeks 3 and 4 a soft diet is consumed, these food stages allow comfortable progression back to solids at one month post-op.
- For those with desk jobs recovery time is usually 2 weeks before returning to work while those with physical jobs may need 3-4 weeks off.
- Exercise is built up gradually with short walks in week 3 after surgery, week 5 is the earliest for a cardio workout as you need to ensure you can consume enough calories, week 6 is the earliest for resistance training in order to avoid a hernia.
See our FAQ’s section for information regarding weight loss surgery.